It’s estimated that more than 30 million Americans suffer from venous disease. Many of those individuals have some type of chronic venous disease, which means that symptoms are persistent or recurring over extended periods of time. Because the venous system runs through the whole body, the symptoms of and locations affected by chronic venous disease can vary. Symptoms can include swelling, restlessness of the legs, pain or cramping, skin discoloration or itching, and ulcers or sores.
Many conservative treatment options exist like compression stockings, exercise, anticoagulants or blood thinning medications, or external compression devices. However, many patients with chronic venous disease find no relief even after these types of treatments.
At UVA Health, we want you to be aware of all treatment options we offer for chronic venous disease. The highly-skilled, sub-specialized interventional radiologists at UVA provide minimally-invasive, x-ray guided venous reconstruction for complex venous disease. Continue reading to learn more about venous reconstruction, which targets structural vein issues and can provide relief for patients with chronic venous disease when conservative treatments are not enough.
Article Reviewed by Minaj Khaja, MD and Brigitte Kelly, BSN, RN, CCRC
Understanding Chronic Deep Venous Disease
Veins are an important part of the vascular system, which carries blood and oxygen throughout your body. Veins are responsible for carrying blood that has circulated in the body back to the heart, and have tiny “one way” valves inside of them that help prevent blood from flowing backward.
There are two main types of veins : superficial veins are the veins just under the surface of your skin. Deep veins exist farther from the body’s surface and are typically closer to your arteries, muscles, and organs.
Most chronic venous disease deals with the deep veins of the body. Exact symptoms will depend on which deep veins are affected. Three deep veins that are commonly affected by venous disease are the Superior Vena Cava (SVC vein), the Inferior Vena Cava (IVC vein), or the Iliac Vein.
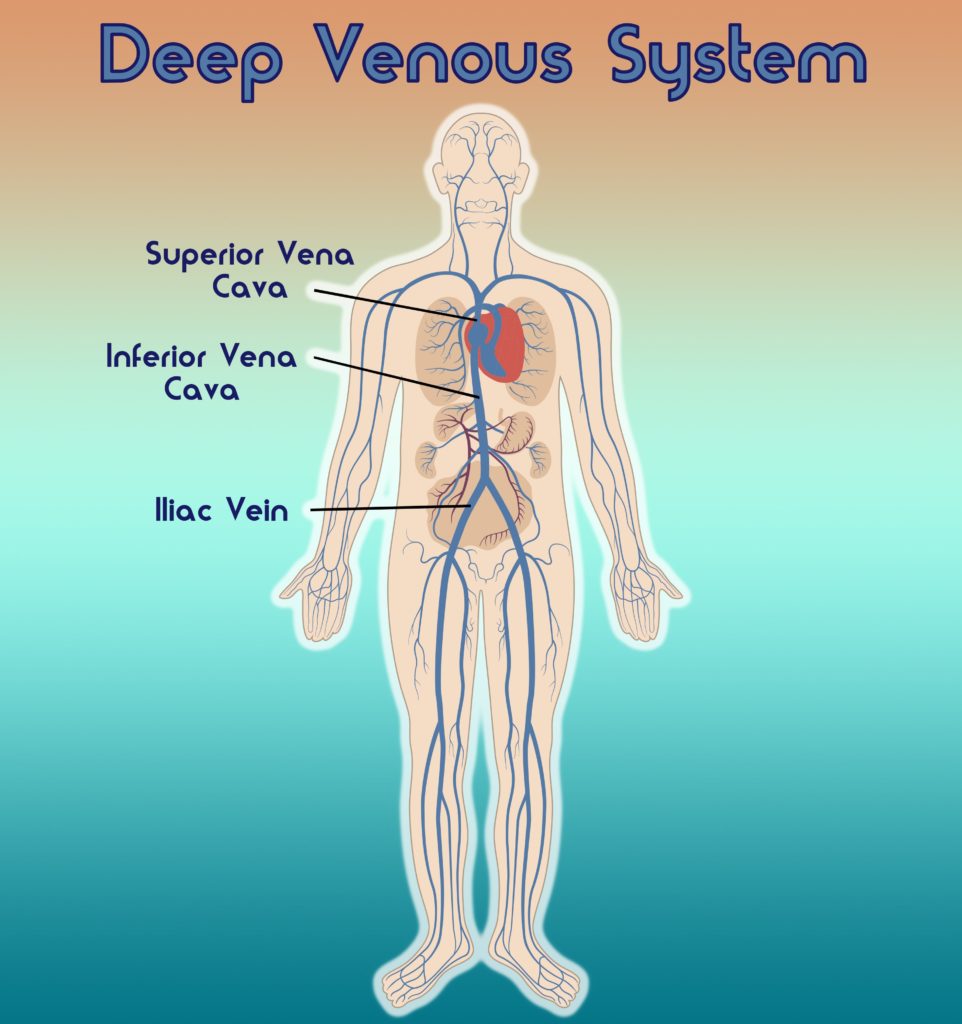
The diagram above shows where each of these veins are located in the body. The superior vena cava or SVC is located above the heart, and its job is to return blood that has circulated from the upper half of the body back to the heart. When someone has what is called SVC syndrome, they may have swelling of the face or arms, headaches, vision problems, difficulty breathing, feelings of passing out, and sometimes internal swelling in the brain or throat.
The inferior vena cava or IVC is the largest vein in the whole body, and is located in the abdomen. The purpose of the IVC is to return blood that has circulated in the lower and middle region of the body (legs, pelvis, abdomen) to the heart. The iliac vein is located in the pelvis and it works to send blood which has circulated in the legs and pelvis to the IVC. The IVC then returns the blood back to the heart.
When a patient has chronic venous disease or a blockage affecting the iliac or IVC vein, they will usually have symptoms in the lower half of their body. This can include symptoms that greatly affect everyday life, such as severe swelling in the legs that makes walking or bending difficult, legs that feel heavy, discoloration of the skin, and painful ulcers that won’t heal.
Risk Factors for Chronic Venous Disease
There are many underlying causes or risk factors for chronic deep venous disease, including:
- History of a blood clot or blood clotting disorder
- Obesity
- History of deep vein thrombosis
- Long periods of standing or sitting (waitstaff, truck drivers, nurses)
- Pregnancy, due to compression of the pelvis
- Smoking
- Being over the age of 50
- Females are more likely to have this condition than men
- Congenital heart disease
- Recent major injury or surgery
- Use of medical devices which involve accessing the venous system, such as pacemakers, central venous lines, or implantable ports
Regardless of the underlying cause or which vein is affected, chronic venous disease causes the tiny one-way valves within veins to weaken. When the valves become weak, they can no longer stop the blood from flowing backward. This means that the veins can no longer effectively carry all the blood back to the heart. This causes some blood to pool or sit in the veins, resulting in increased pressure to the wall of the vein. This increased venous pressure is what causes symptoms to present such as swelling, aching, and cramping. If pressure in the veins continues to increase over time, the walls of the vein become weak and blood can leak into the surrounding tissue causing discoloration of the skin, annoying itching, and even ulcers or sores.

How Interventional Radiologists Perform Deep Vein Reconstruction
As detailed above, chronic venous disease is just as complex as the branching venous system throughout our bodies. This means that there is no one way to solve venous disease.
While there are many conservative treatments for venous disease such as compression, exercise, or blood thinning medications, most of these do not address the structural issues within the veins that keep them from functioning properly. For this reason, interventional radiologists have a well-rounded approach to reconstructing deep veins, catered to each patient’s specific and complex needs.
All of the methods interventional radiologists use for venous reconstruction are performed under image-guidance, meaning they use fluoroscopy (a type of continuous x-ray imaging) to see inside the patient and get a close-up view of their veins. This allows physicians to insert catheters into the veins through tiny incisions, so there is no significant tissue damage to the body. The techniques used to reconstruct veins include:
- Venopasty– a balloon is inflated inside a narrowed vein to widen the walls of the vein so that blood can flow properly.
- Stenting– a small metal, mesh tube is inserted into a narrowed vein to support and open the walls of the vein so that blood can pass through.
- Thrombolysis– a special catheter is placed inside of a blood clot that is blocking blood flow through the vein, and a blood clot “busting” medication is delivered to the clot to dissolve it.
- Mechanical Thrombectomy– a special device is guided to the site of the blood clot where it is used to mechanically break up the clot and remove the remaining pieces.
- IVC Filters– a special filter is positioned in the Inferior Vena Cava where it can trap large blood clots to prevent them from reaching the heart or lungs. Most IVC filters are removed once a blood clot is cleared.
Once an interventional radiologist has assessed the unique structural needs of the veins, the methods above may be used separately or in combination to reconstruct veins and restore normal blood flow to the body. This procedure can last anywhere from 2 to 12 hours, depending on the complexity of the vein dysfunction and complexity of disease.
The Interventional Radiologists at UVA Health have extensive knowledge of the vascular system and are specially trained to perform deep vein reconstruction. This type of structural vein treatment has proven results and brings longer-lasting relief for venous disease. If, like millions of other Americans, you have tried other treatments for your chronic venous disease and are still suffering, talk with your doctor about a referral to UVA Interventional Radiology today.



